A Discussion of Evolving Modalities in Medical Education for Anesthesiology Residents
A Discussion of Evolving Modalities in Medical Education for Anesthesiology Residents
 Rahul Kukreja |
 Jeremy Tang M.D. |
 Benjamin Landgraf M.D. |
 Alopi Patel M.D. |
The field of education in anesthesiology has undergone significant changes in recent years. Anesthesiology trainees now engage in many different learning styles and use a multitude of educational resources. Understanding and incorporating these various learning modalities is important not only for effective residency training but also for improving patient outcomes, quality of care, and clinical revenue.1,2
Podcasts
In the past, residents typically engaged in didactic sessions with in-person lectures to gain relevant knowledge about specific topics that appear on exams and clinical encounters.3 However, non-synchronous forms of audio such as podcasts or pre-recorded lectures have become popular among medical trainees.4,5 In a study of anesthesiology residents and medical students examining the effects of supplementing traditional didactic lectures with a podcast module, participants were either placed in groups that only had an in-person lecture or had a pre-lecture podcast about instructions for evaluating electroencephalograms (EEG). Participants who listened to the podcast had greater increases in scores from their baseline abilities compared to those who only had traditional lecture sessions without any podcast modules. Additionally, those with previous experience listening to podcasts had greater gains in scores compared to those with less experience. 6 Similarly, a survey of Canadian anesthesiology residents found that around 60% of respondents were individually using medical podcasts to supplement their education and over 70% cited that podcasts allowed them to review materials at any time they wanted for self-directed learning.7 Another study measured learner attention, knowledge retention, and exam performance in anesthesiology residents and medical students from studying with podcasts compared to traditional learning modalities. They found that participants had increased learning attention measured through EEG, better exam scores, and higher preference for listening to podcasts compared to reading textbooks.8 The higher knowledge retention, performance, and preference towards podcasts as an educational modality across multiple studies indicates the benefit of incorporating podcasts into more traditional curriculums.
Social Media Platforms
Anesthesiology residents also use various forms of digital media to supplement their education. Platforms such as X (formally known as Twitter), blogs, and podcasts were among the most commonly used. A systematic review evaluating the use of social media in medical education found that Twitter and blogs specifically help discuss clinical concepts and easily share relevant medical information. Users are also able to find specific anesthesiology topics based on accounts they follow or use hashtags to filter for related posts. These functionalities may explain why the majority of residents believe that Twitter enhances their residency training. 9,10 11
YouTube is another widely used form of video-based media that has content related to anesthesiology training. New York School of Regional Anesthesia (NYSORA) and the Regional Anesthesiology and Acute Pain Medicine pages are two popular YouTube channels, hosted by physicians that have garnered tens of thousands of followers, with educational videos focusing on procedures and clinical concepts. While studies find that learners believe these types of YouTube videos are useful due to their format, accessibility, and self-pacing features, a disadvantage is that videos on YouTube are technically not peer-reviewed nor frequently evaluated for educational standards and misinformation. With increasing preferences towards using these digital and social media platforms as educational supplements, educators can consider employing these platforms more often to engage the broader academic community while exploring ways to validate and verify the information on these newer modalities.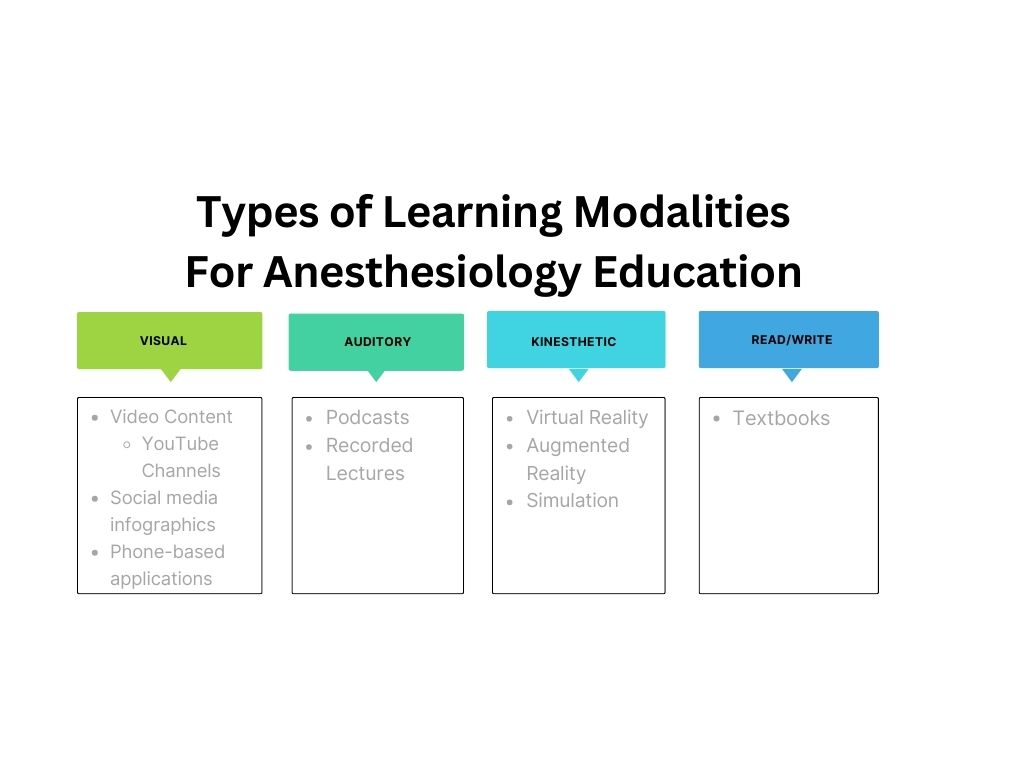
Simulation
Simulation has been reported to be a part of resident education for over 80 years, and it continues to be integrated into medical education as an opportunity to practice procedures in situations that simulate real patients. These simulation-based settings allow for learning in a safe manner as well as allow educators to evaluate residents and identify specific difficulties residents may be experiencing.12,13 Currently, many simulation trainings use realistic interactive mannequins or three-dimensional models as training modalities. These realistic simulations allow residents to improve their skills in procedures that are commonly encountered or notoriously challenging. In a study of pediatric anesthesia attendings, fellows, and rotating residents, participants watched a video on ultrasound-guided intravenous catheter insertion and then underwent deliberate practice on a three-dimensional simulator until they were able to achieve a passing standard. While only 21% of participants met a minimum passing standard on a pre-test, 96% of participants met the passing standard on their first post-test, elucidating the positive impact of realistic simulation on procedural skills.14
Virtual/Augmented Reality
With technological advances in recent years, simulation modalities have progressed further to incorporate virtual (VR) and augmented reality (AR). The various forms of VR and AR simulation modalities include only computer screen-based trainings, VR procedural systems, and immersive headset-based simulations.15 Screen-based programs allow learners to go through patient cases with multimedia and visual representations of commonly encountered clinical problems in which participants can access information, make corresponding decisions as they arise on the screen, and visualize the effect of their decisions or the evolving clinical case. These screen-based simulations allow trainees to improve clinical reasoning and decision-making with great accessibility given that the only requirement is a computer-based screen. However, they do not allow for the development of procedural, motor, and tactile skills that require immense practice to increase skill and confidence. 16
VR procedural simulation systems allow learners to practice with tools replicated from those used in clinical settings to allow for high-fidelity training. Airway management and bronchoscopy are the most common VR procedural simulations used in anesthesia education. ORSIM is a VR bronchoscopy simulator that includes a replica video bronchoscope, a desktop sensor module, and a laptop computer that reproduces anatomical reality for a variety of airway types and provides feedback, measurements, and relevant clinical data.17 A study of anesthesiologists and anesthetic technicians with ranges of novice to expert level experience found that there were significant differences between simulation performances positively correlated with experience and expertise, showing the validity and reliability of VR procedural systems like ORSIM.18 Unfortunately, there are very few validated VR bronchoscopy simulators available in the market and most of them are at high costs ranging from $25,000 to $100,000, causing a large barrier to entry for wide-spread use.19
There are numerous learning modalities available to anesthesia trainees that can cater to every type of learning. Since traditional educational methods alone may not fully leverage the technological advancements and most efficient forms of information delivery, residency programs should embrace these new educational tools to advance the field of anesthesiology and maximize anesthesia residents’ abilities to deliver the highest level of patient care throughout each stage of their training. Further work should be done to evaluate and productively incorporate these relatively new modalities given their scarcity of research and real-world applications.
- Turner BC, Tsai MH, Black IH, Mathews DM, Adams DC. Observations: clinical revenue directly attributable to anesthesiology residents. J Grad Med Educ. Jun 2014;6(2):384. doi:10.4300/jgme-d-13-00419.1
- van der Leeuw RM, Lombarts KM, Arah OA, Heineman MJ. A systematic review of the effects of residency training on patient outcomes. BMC Med. Jun 28 2012;10:65. doi:10.1186/1741-7015-10-65
- Martinelli SM, Chen F, DiLorenzo AN, et al. Results of a Flipped Classroom Teaching Approach in Anesthesiology Residents. J Grad Med Educ. Aug 2017;9(4):485-490. doi:10.4300/jgme-d-17-00128.1
- Cadogan M, Thoma B, Chan TM, Lin M. Free Open Access Meducation (FOAM): the rise of emergency medicine and critical care blogs and podcasts (2002-2013). Emerg Med J. Oct 2014;31(e1):e76-7. doi:10.1136/emermed-2013-203502
- Kiernan MA, Mitchell BG, Russo PL. The power of podcasts: Exploring the endless possibilities of audio education and information in medicine, healthcare epidemiology, and antimicrobial stewardship. Antimicrob Steward Healthc Epidemiol. 2023;3(1):e98. doi:10.1017/ash.2023.178
- Vasilopoulos T, Chau DF, Bensalem-Owen M, Cibula JE, Fahy BG. Prior Podcast Experience Moderates Improvement in Electroencephalography Evaluation After Educational Podcast Module. Anesth Analg. Sep 2015;121(3):791-797. doi:10.1213/ane.0000000000000681
- Matava CT, Rosen D, Siu E, Bould DM. eLearning among Canadian anesthesia residents: a survey of podcast use and content needs. BMC Med Educ. Apr 23 2013;13:59. doi:10.1186/1472-6920-13-59
- Wolpaw J, Ozsoy S, Berenholtz S, et al. A Multimodal Evaluation of Podcast Learning, Retention, and Electroencephalographically Measured Attention in Medical Trainees. Cureus. Nov 2022;14(11):e31289. doi:10.7759/cureus.31289
- Sterling M, Leung P, Wright D, Bishop TF. The Use of Social Media in Graduate Medical Education: A Systematic Review. Acad Med. Jul 2017;92(7):1043-1056. doi:10.1097/acm.0000000000001617
- Mulaikal TA, Helou MF, Martinelli SM. Training the next generation of anesthesiologists. Int Anesthesiol Clin. Fall 2020;58(4):23-30. doi:10.1097/aia.0000000000000299
- Kumar AH, Udani AD, Mariano ER. The future of education in anesthesiology is social. Int Anesthesiol Clin. Fall 2020;58(4):52-57. doi:10.1097/aia.0000000000000287
- Blum RH, Boulet JR, Cooper JB, Muret-Wagstaff SL. Simulation-based assessment to identify critical gaps in safe anesthesia resident performance. Anesthesiology. Jan 2014;120(1):129-41. doi:10.1097/aln.0000000000000055
- Yunoki K, Sakai T. The role of simulation training in anesthesiology resident education. J Anesth. Jun 2018;32(3):425-433. doi:10.1007/s00540-018-2483-y
- Ballard HA, Tsao M, Robles A, Phillips M, Hajduk J, Feinglass J, Barsuk JH. Use of a simulation-based mastery learning curriculum to improve ultrasound-guided vascular access skills of pediatric anesthesiologists. Paediatr Anaesth. Nov 2020;30(11):1204-1210. doi:10.1111/pan.13953
- Huang VW, Jones CB, Gomez ED. State of the art of virtual reality simulation in anesthesia. Int Anesthesiol Clin. Fall 2020;58(4):31-35. doi:10.1097/aia.0000000000000298
- Rosenberg M. Simulation Technology in Anesthesiology. Anesth Prog. Dec 1 2021;68(4):238-241. doi:10.2344/0003-3006-68.4.238
- Vieira LMN, Camargos PAM, Ibiapina CDC. Bronchoscopy simulation training in the post-pandemic world. J Bras Pneumol. 2022;48(3):e20210361. doi:10.36416/1806-3756/e20210361
- Baker PA, Weller JM, Baker MJ, Hounsell GL, Scott J, Gardiner PJ, Thompson JM. Evaluating the ORSIM® simulator for assessment of anaesthetists' skills in flexible bronchoscopy: aspects of validity and reliability. Br J Anaesth. Sep 2016;117 Suppl 1:i87-i91. doi:10.1093/bja/aew059
- Casso G, Schoettker P, Savoldelli GL, Azzola A, Cassina T. Development and Initial Evaluation of a Novel, Ultraportable, Virtual Reality Bronchoscopy Simulator: The Computer Airway Simulation System. Anesth Analg. Nov 2019;129(5):1258-1264. doi:10.1213/ane.0000000000003316
About the Authors
- Rahul Kukreja is a 3rd year medical student at Rutgers-Robert Wood Johnson Medical School
- Dr. Jeremy Tang is a CA2 at Rutgers-Robert Wood Johnson Medical School
- Dr. Benjamin Landgraf and Dr. Alopi Patel are faculty at Rutgers-Robert Wood Johnson Medical School


